How Worried Should We Be About Bird Flu?
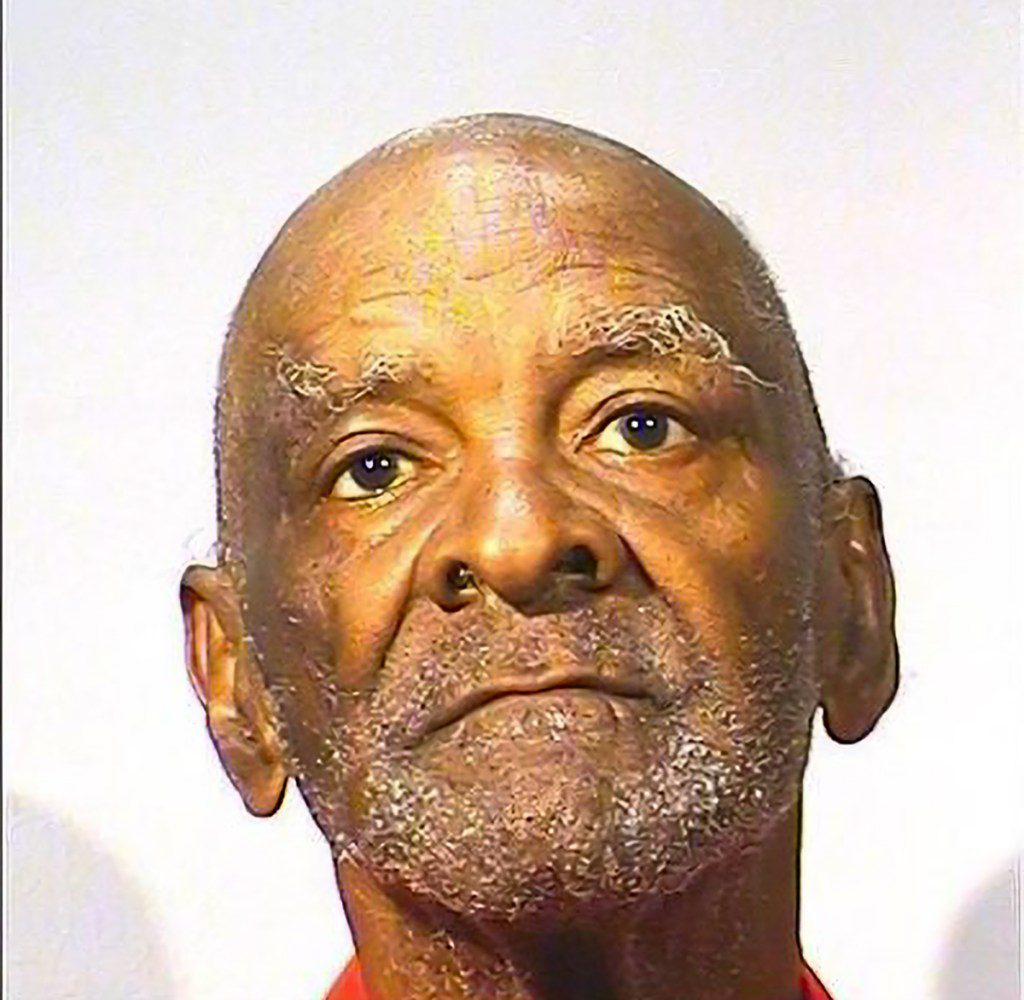
Earlier this month, the Centers for Disease Control and Prevention (CDC) announced that a Louisiana resident had been hospitalized with the first severe case of avian influenza — also known as “bird flu” — in humans. A total of 65 other people in the United States had contracted the H5N1 virus, though their symptoms had been relatively mild in comparison. While the CDC is still investigating the precise source of the infection, the agency determined that the Louisiana patient was exposed to sick and dead birds in backyard poultry flocks, and the infection is not the result of human-to-human transmission.
And that’s only one of the most recent headlines related to ongoing bird flu outbreaks across the country — some of which pertain to hot-button political issues like raw milk and the price of eggs. But what, exactly, is going on with bird flu? How widespread is it? Are we looking at the next pandemic, or do public health officials believe the virus can be contained to a handful of isolated cases in humans? Here’s what we know so far.
What is bird flu?
“Bird flu” is the disease that results from contracting Avian influenza A viruses, which spread between birds and other animals through saliva, feces, and mucus. Currently, one subtype of avian influenza A viruses, H5N1, is being transmitted around the world and causing outbreaks in the United States. In addition to “H5N1” and “avian flu,” the current iteration of bird flu is also known as “highly pathogenic avian influenza” (HPAI), which refers to a strain of H5N1 that’s especially likely to cause disease.
Avian influenza A viruses occur naturally in wild aquatic birds, but can also infect domestic poultry and other bird and animal species. The H5N1 virus has recently spread to chickens, turkeys, dairy cattle, pigs, cats, and minks in the U.S., as well as foxes, sea lions, and sea elephants outside of the country.
So far, there have been 66 confirmed human cases of bird flu, all but three of which were the result of people coming into contact with infected dairy cattle or poultry. (One case came from exposure to an animal that’s not livestock; the sources of two cases remain unknown.) Currently, bird flu isn’t spreading from person to person, but researchers and public health officials are tracking and monitoring the human cases — and how they were transmitted — closely.
How many animals have been infected?
With bird flu being widespread among wild birds, all eyes are on infection rates in livestock — poultry and dairy cattle in particular — because humans are more likely to come in contact with and consume farm animals and animal products. (More on those safety concerns in a minute.) In February 2022, the Animal and Plant Health Inspection Service (APHIS), an agency of the U.S. Department of Agriculture (USDA), confirmed the first cases of this highly pathogenic strain of the H5N1 virus in commercial poultry. Since then, it has resulted in the deaths of 128.91 million birds in a total of 1,349 flocks of commercial and backyard poultry.
Infections tend to be more common in the spring and fall, when wild birds transmit it during and after their migration. And while this was the case in October and November, H5N1 spread even more rapidly in December, when 15.56 million birds were wiped out, compared to 4.37 million birds in October, and 6.9 million birds in November, according to the APHIS. (For perspective, there are more than 378.5 million egg-laying chickens in the United States, and in 2023, more than 9.4 billion broiler chickens and 218 million turkeys were processed.)
Meanwhile, the virus was first detected in dairy cattle in Texas and Kansas in March; by Dec. 25, it had been confirmed in 891 herds in 16 states, out of the country’s approximately 26,000 licensed dairy herds. Most cases have been in the West, with California serving as the epicenter of the outbreak, with 446 newly affected herds in October and November alone.
What does bird flu have to do with raw milk and egg prices?
In November, samples of raw milk from California were found to contain the H5N1 virus — an especially troubling development considering its increase in popularity over the past year. However, based on the limited research and information available, it’s still unclear whether the virus can be transmitted to people through the consumption of raw milk and unpasteurized dairy products, like cheese, according to the CDC. We do, however, know that drinking raw milk can lead to infection in cats. Of the dozens of felines infected by the virus since March, some contracted H5N1 through raw milk, while at least one — which subsequently died — got it from eating raw frozen pet food.
Thanks to a federal order the USDA issued earlier this month requiring the collection and testing of raw milk samples from around the country, agriculture and public health officials are now able to monitor the nation’s milk supply and dairy herds. We also have a better idea of how long it could stick around: a new study out of Stanford University found that influenza virus can remain infectious in refrigerated raw milk for up to five days. Raw milk is unpasteurized, meaning that it hasn’t been heated up to a temperature that kills potentially dangerous pathogens.
Milk’s not the only grocery staple bird flu has affected: it’s also behind recent increases in the cost of eggs. When H5N1 is detected in hens, the entire flock is euthanized, decreasing the country’s supply of eggs, and driving up the price of a dozen.
How worried should we be about bird flu?
According to the CDC, the immediate risk to public health from bird flu remains low. People who work with poultry and dairy cattle have a greater chance of being exposed to the virus and getting sick. “[Bird flu] is not yet a threat to everyday people who are not in close contact with affected animals, such as dairy cattle, poultry and wild birds, and we have not seen any human-to-human transmission of the virus,” Jonathan Grein, MD, director of hospital epidemiology at Cedars-Sinai and head of the medical center’s Special Pathogens Response Team explained in a statement.
But just because the CDC doesn’t view bird flu as a major risk to public health at the moment, it doesn’t mean that we shouldn’t take it seriously. We know from previous outbreaks that while some infections come with mild symptoms — or none at all — others can result in severe illness, complications, or even death. We also know that avian influenza A viruses like H5N1 are unlike the average seasonal variety that circulate each winter. “They have the potential to cause a pandemic in people if they were to gain the ability to more easily infect and spread efficiently between people because people have little pre-existing immunity to these viruses,” per the CDC.
Plus, as we learned from Covid, viruses have a tendency to change over time — and there’s already evidence of that happening. After sequencing viral specimens collected from the severely ill patient in Louisiana, the CDC announced on Thursday that genetic mutations had been identified in some of the samples. The mutations appear to have emerged in the patient after infection, and have the potential to make the virus spread more easily among people — a development the agency called “concerning.”
So, are we ready should bird flu ramp up? According to the APHIS, “the United States has the strongest avian influenza surveillance program in the world,” and despite the recently discovered mutations of the virus, the CDC asserts that the risk to the general public is still low. Meanwhile, some public health experts, like Amesh Adalja, MD, of the Johns Hopkins Center for Health Security, haven’t been impressed with the government’s response to H5N1 so far, and don’t exactly have confidence in the incoming administration. “I don’t think H5N1 has been managed very well in the Biden-Harris administration, and probably will only get worse during the Trump administration, if we can judge by some of their Covid policies, as well as some of the people who are going to be put in charge of agencies,” he told MedPage Today.
How can bird flu be prevented in humans?
Being exposed to sick or dead infected animals is the main way to get bird flu, according to the CDC. To avoid contracting the virus, try to steer clear of chickens, cows, and other infected or potentially infected livestock or wild animals whenever possible. If it’s not, the CDC recommends wearing personal protective equipment (PPE). Unfortunately, this year’s flu shot probably doesn’t offer any protection against bird flu, Grein noted.
This should go without saying, but be sure to fully cook poultry, eggs, and beef to kill viruses and bacteria. And no matter what the presumptive incoming head of the Department of Health and Human Services says, only consume pasteurized milk and dairy products.
While the CDC has stressed that bird flu doesn’t put public health at immediate risk, it’s still important to take it seriously. “We’re concerned that this virus now spreads more readily across mammals — cattle in particular — and as this virus mutates and adapts, it has the potential to spread even more easily,” Grein said. “We must remain vigilant.”