How Could a Girl in Perfect Health Come So Close to Dying?
The day I almost died began with a bang: Our plane dropped out of the sky. It was the kind of shock you hear with your gut, not your ears — the plane fell 10,000 feet. Birds, said the flight attendant, trying to calm us. Birds flew into our engine and we needed to land.
I was on a morning flight with a hundred girls, coming home from Camp Vega in southern Maine. It was our last day together after eight glorious summers, and we’d stayed up all hours replaying the sweetest months of our lives. We’d boarded the plane at 8 a.m. and were hunched over our cell phones when the plane plunged a half hour later. Somehow, my phone rang in mid-air; it was my mother calling. “Something’s wrong with the engine,” I told her. “We’re being diverted to [Bradley Airport in] Connecticut because we need a longer runway.” My mom, a world-class worrier, did her best not to panic. “Your friends’ moms and I will arrange a van to meet you.”
It wasn’t till we landed that I started feeling ill. Stuck in my seat — we had no gate to park at — my body suddenly started to cook. Nauseous, I begged the flight attendants to let me off. They allowed me and my friend to exit — she was nauseous, too — but made us wait at the top of the rolling staircase. We were out there 20 minutes, heaving over the side rail. When the shuttle finally came and brought us to the hangar, I turned pale and passed out in my seat. By luck, there was an ambulance standing by.
But “luck” doesn’t begin to describe the series of breaks that saved me on the morning of August 11, 2022. Had those birds not hit the plane and diverted us to Connecticut; had there not been EMTs there in case we crash-landed; had I gotten in the van that my mother hired to drive me and six of my girlfriends to Long Island — I’d have surely gone to sleep and not woken up. Because that’s what happens to an otherwise healthy girl who ignores the splotchy rash on her leg. Your body temperature spikes, your blood pressure plummets, and then your heart stops beating. By the time your friends notice that you’re dying, not napping, it’s too late to wake you or get help.
I couldn’t stay awake in the ambulance, passing in and out of consciousness. At the hospital — Connecticut Children’s in Hartford — they put me on a gurney and flushed me full of fluids. I began to feel better and got some saltine crackers down; they were the first thing in my stomach since the night before. My parents got to the hospital just after noon, having raced three hours from Long Island. Though the nurse told my mother I was ready for discharge, I was still fading in and out of focus. Then, as they were talking, my eyes rolled back; everything jump-scared to black. My blood pressure flatlined, cutting blood flow to my organs and robbing my brain of oxygen for almost a minute.
Nurses and doctors raced to revive me. The ER chief, Dr. James Wiley, yelled, “What was wrong with her before she got here?” My mother had no clue — she hadn’t seen me in weeks — so she frantically called my friends in the van. Two of them mentioned the rash on my leg, and that it had kept me from water-skiing. Wiley ordered epinephrine, a stimulant to start the heart, and examined my inner thigh. “She has an infection shutting down her whole body,” he shouted. “Does she have a tampon in?” “Yes, but why?” said my mom. “She always changes it before she’s supposed to.” “Doesn’t matter,” he said. “We have to get it out of her. I think this might be toxic shock.”
The next five days were a blur to me. I’d sleep for 24 hours, wake up and text my girlfriends, then sink into another long swoon. There were multiple IVs in both my arms, pushing a cocktail of antibiotics through my system. Only one of them, Clindamycin, was actually working, though — and I was allergic to it. No matter how much lotion I rubbed on my arms, they felt like scratching posts. Making matters worse, I wasn’t getting better. Three nights in, I was still on epinephrine — and my vitals plunged both times they took me off it. On the fourth night, the infectious-disease doctor stopped by. “We have to try again,” he told my parents. “It’s too dangerous to keep her on it.” This time, they weaned me off, bit by bit — and my blood pressure and heart rate held steady.
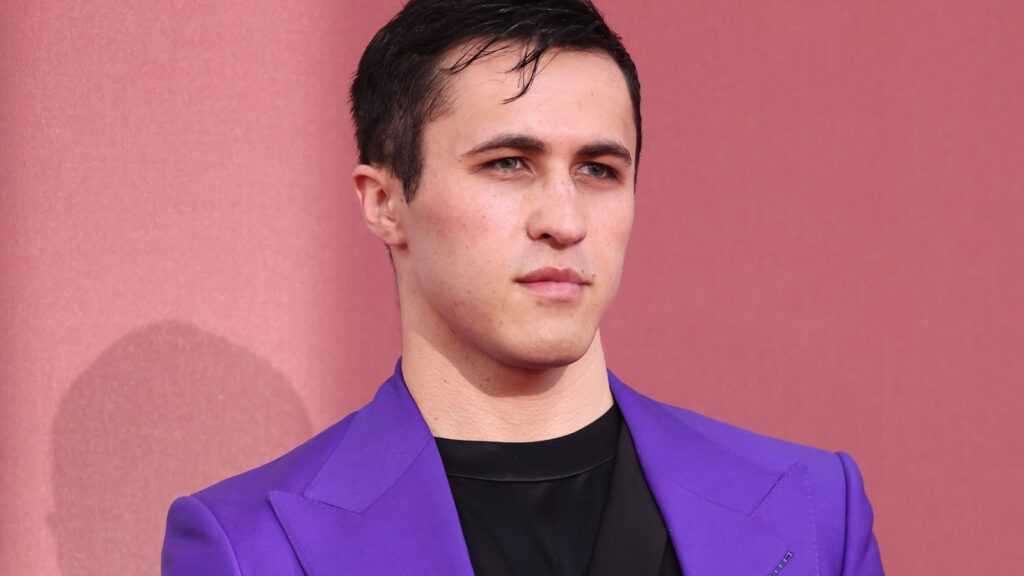
The author in the hospital
Courtesy of Audrey Kirdar
By day five, the infection was contained enough that I was able to clear protocols and go home. I was given a two-week course of Clindamycin and told never to use tampons again, for fear of re-infection. In fact, even if I did everything right for the rest of my life, I still stood a 40 percent chance of getting sepsis again. As we prepared to leave, my test results came back, confirming menstrual toxic shock syndrome, or mTSS. “That was my first guess, because I’m old enough to remember the Eighties,” said Dr. Wiley, referring to a major spike in toxic shock cases among American girls and women. That surge in cases terrified the public, and forced tampon manufacturers to reformulate their products. They cut back on chemical additives in their super-absorbent styles, and posted warning labels in or on the boxes.
Dr. Wiley told my parents how lucky I’d been, using the phrase “divine intervention.” If I hadn’t been as young and healthy as I was; if I hadn’t come to a Level One trauma center; and if I’d gotten on that van with my summer camp friends, the outcome would have been “much, much worse,” he said. Organ failure, brain damage, even sudden death: Any or all of that could have happened in short order. He said that mTSS wasn’t fully understood — but that I was at peak risk for it. Cases are most common in menstruating females between the ages of 15 and 25. He mentioned tampons as a risk factor if left in too long — meaning, more than six to eight hours. I said I faithfully changed mine before the six-hour limit: It was the one thing I’d learned in seventh-grade health-ed class. He shrugged and said something about other risk factors: a pre-existing infection or an immunological weakness. But by that point, I wasn’t really listening anymore. I just wanted to go home.
IF SNAKES HAD FEET, they’d probably feel like mine when I got out of the hospital. My soles cracked and blistered till the skin peeled off — then did so again and again. Same with my palms; they callused and chapped, either from the toxins or antibiotics. Dr. Wiley had warned me that my skin would shed. Still, I was surprised — and shocked. So shocked, in fact, that I said nothing to my friends — I couldn’t even explain it to myself. How could a girl in perfect health have come so close to dying? I scoured the internet and read everything I could on the subject of mTSS. But most of the links were 40 years old. Even recent entries on WebMD were too vague to give me comfort.
Since I couldn’t use tampons, my doctor prescribed birth control pills to reduce the frequency of my periods. But then I had to explain to my girlfriends on sleepovers why I was on the pill. I told them I’d caught sepsis, that it had very nearly killed me, and that the pill helped me avoid reinfection. But I left out any mention of my vaginal tract; somehow, that felt too personal to share, even with girls I’d known half my life. Because that’s the thing about being 15 and female: You’d sooner stick steak-knives down your throat than say the words vaginal tract to friends.
Still, I needed answers to the questions in my head. I’d gotten no info in middle school health-ed about mTSS from my teachers. Even if it was offered, I’d have been too embarrassed to hear it in a room full of boys. My mother, the professional worrier, also had questions. She booked us an appointment with an infectious-disease expert at a top-tier hospital in Manhattan. That doctor couldn’t tell me why I’d come down with mTSS, though the fact that I’d been wearing a super-absorbent style increased my risk, she said. I asked her if any products were safe for me to use. She contradicted Dr. Wiley, saying most of them were fine, so long as they weren’t left in past eight hours. I walked out as flummoxed as when I’d entered. Was there no one in the field who could shed light on my plight — and why was this so poorly understood?
Meanwhile, I had a life to live. In the summer of ’23, I toured Europe with some friends and met up with other kids we didn’t know. I wound up telling one of those girls the story of my ordeal, and for the first time left nothing out. She was stunned to hear about toxic shock and insisted I tell her girlfriends. By the end of the trip, I’d told a dozen girls; it got easier each time I told it. Those girls either had never heard of mTSS, or thought it was ancient history. By the time I flew back home, I knew I had a duty: to tell every girl who’d listen about toxic shock.
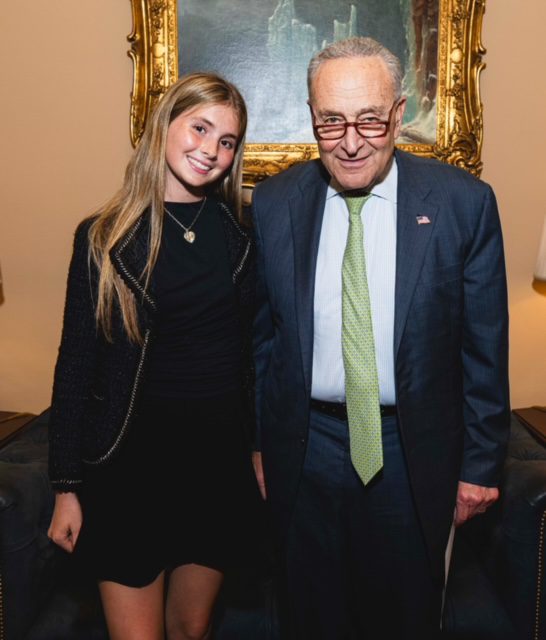
With Senator Chuck Schumer
Courtesy of Audrey Kirdar
So I built a website called teachschoolsshock.com around an essay I’d written about my illness, and filled it out with links to other personal accounts of toxic shock. One of those links was to a site called dontshockme.org. It was created by Dawn Massabni, a mother in New Jersey who lost her teenage daughter Madalyn to mTSS in 2017.
“Maddy was home from college for her birthday,” says Massabni, “and came down with what I thought was a stomach bug.” Massabni sent her daughter to bed, and Maddy seemed to rally the next day. But the following morning, she got out of bed and collapsed. Her heart stopped beating while the ambulance was on its way. “She was dead 36 hours after her 19th birthday,” says Massabni, who can’t speak of Maddy without weeping. “I still see it like it was yesterday, six years later.”
Blood work confirmed the cause of death: Maddy died of toxic shock. “I swore to her in the hospital that I would do everything in my power to make this right to her,” says Massabni. She launched dontshockme.org in 2018 to inform girls and young women about mTSS. She successfully pushed the schools in her hometown of Rumson to make mTSS lessons compulsory for girls 10 and up. She’s also waging a push for a bill called Madalyn’s Law. It would make those lessons mandatory throughout New Jersey, and force bars and restaurants to post warning signs on tampon vending machines in women’s restrooms. She invited me to speak at an event in her state; I told her I’d be honored to do so.
Then, last fall, I got lucky again. I was introduced to a brilliant specialist at the hospital that saved my life. Dr. Juan Salazar, the chairman of the Infectious Disease Department at Connecticut Children’s, had the answers I’d been seeking for over a year. “What happened to you is, sadly, typical in mTSS,” he explained. “It favors young, healthy girls — even the ones who faithfully change tampons.” If “just the right strain of staph bacteria” is lurking, he said, then taking out a tampon and inserting a new one can push the infection down deeper. At that point, said Salazar, a vicious cycle begins. The staph infection rockets throughout the body and triggers the release of a “super-toxin.” That super-toxin sends the immune system into hyper-drive, wherein T-cells attack the body with cytokines, and then your blood pressure crashes. With little or no blood flow, your organs stop working, and the oxygen shortage shuts down your brain. “Before you know it, your whole body switches off,” he said.
Armed with that revelation, I set my sights higher. This spring, I lobbied legislators in New York State to pass a bill like Madalyn’s Law, and testified in front of a thousand physicians about my toxic shock ordeal. For many of them, this was new information, the first time they’d heard from a survivor. Even among doctors, there’s a huge gap in their training — maybe because there hasn’t been an outbreak in 40 years. It’s my goal to help fill in that gap, joining forces with Massabni on a second bill that would up-train healthcare workers. It’s so important for patients and doctors to know the signs of mTSS, says Massabni. Because “once you’re sick,” she adds, it’s a very “thin line between living and dying.”